In a world where their pain and experiences are so often invisible, people living with chronic pain yearn to be seen and heard. The endless search for diagnoses, treatment, and emotional support can leave people depressed, exhausted, and isolated. If you have ever treated a person who lives with chronic pain, you may have been shocked by the degree to which it impacts every aspect of their life and personal identity. As a therapist, you have the ability to give your clients the visibility, validation, and tools they need to move forward, alongside their struggles.
Today, it is no secret that emotional and physical wellbeing are inextricably connected. On a physiological and neurological level, what happens in our bodies affects our brains and emotions – and vice versa. Unfortunately, this fact has not trickled down to the world of chronic pain treatment, a field that stumps even most medical professionals.
Consequently, people who live with chronic pain often fall through the cracks; their medical treatments do not take into account the mental health impacts, while their therapeutic processes often do not place enough focus on physical experiences. At Live the Pain, we ensure that people living with chronic pain receive the physical and emotional support they need from expert professionals that understand the complex relationship between the two.
This article briefly introduces several areas where the interconnectedness of these aspects of the chronic pain experience are clear. While it is not possible to fully explore these complex topics within the scope of this article, beginning to deepen your understanding of the chronic pain experience will enable you to create a safe environment and provide more effective, holistic treatment for your clients. If you are interested in learning more about this field, see our upcoming professional training courses for therapists.
Traumatizing aspects of the chronic pain experience
While most people associate trauma with war and sexual abuse, trauma is actually a natural response to a wide variety of difficult life events. According to recent research, 25% of people living with chronic pain also struggle with PTSD. Pain-related trauma can stem from many different sources, including invasive treatments, negative interactions with medical professionals, and the source of the pain, such as an illness or accident. In addition, the physical pain itself can be traumatic. As such, people living with chronic pain may exist in a constant state of emergency, always fearing the next pain flareup that could attack at any moment. In order to effectively treat people living with chronic pain, both physically and emotionally, it is critical to employ trauma-informed treatment approaches.
The secondary trauma of pain disclosures
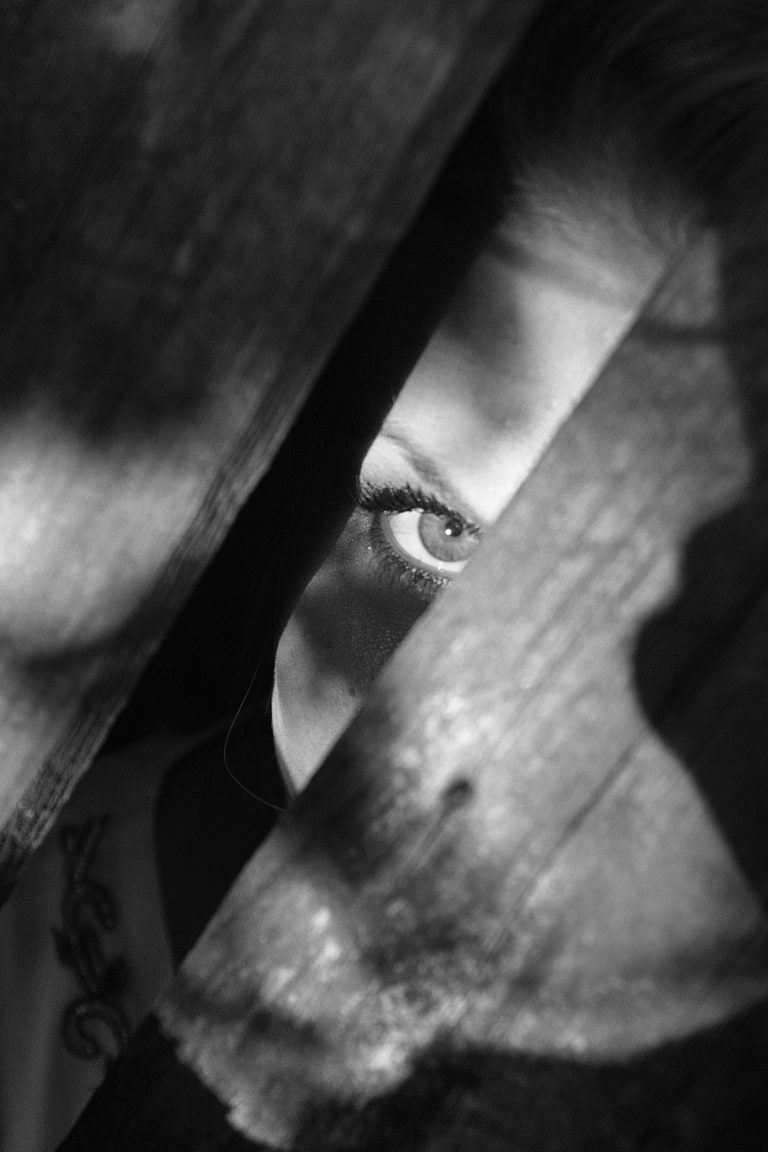
In addition to the sources of trauma listed above, many people living with chronic pain also face the secondary trauma that emerges from negative external responses to pain disclosure. Because chronic pain is often invisible, immeasurable, and unpredictable, it can be very difficult for people to understand, including doctors, therapists, family, friends, coworkers, and strangers. When people living with chronic pain divulge their vulnerable experiences to others, they are often met with doubt, suspicion, and even blame. Especially when they come from trusted loved ones, these painful reactions can damage core relationships and support networks, increasing isolation. Furthermore, it is not uncommon for people to internalize these doubts, questioning their own sanity or the role they may have played in their own pain. Even if these thoughts are completely baseless, they can destroy a person’s sense of self. By validating your clients’ experiences and helping them learn to trust themselves, you can assist them in rebuilding their relationships with themselves and those around them.
The impact of chronic pain on relationships
Beyond the gaslighting and doubt from others, chronic pain can have a significant effect on interpersonal relationships. People living with chronic pain are often ashamed of how their limitations affect others. They may fear becoming a burden or facing rejection if they share or ask for too much. These fears are often based on painful life experiences, where their needs and feelings were not respected. Consequently, people living with chronic pain may withdraw from others, build up protective walls, or refrain from requesting the help they need. Alternatively, they may live a double life, suffering in silence while pretending that everything is fine in order to gain the social acceptance and sense of normalcy they desire. All of these factors can make it difficult for people living with chronic pain to enjoy authentic relationships, while causing tremendous pain, loneliness, and even secondary trauma. Guiding your clients through the process of recognizing toxic relationships, identifying their needs, and communicating them in a healthy manner will enable them to build healthy, mutual relationships.
Anxiety and depression in the chronic pain experience
According to research, 84% of people living with chronic pain also struggle with depression and 60% with anxiety. These staggering statistics stem from a wide variety of factors, including the unpredictability of the chronic pain experience and the frustrating search for accurate diagnoses and effective treatments. People may feel overwhelmed and helpless in the face of their pain. Anxiety, depression, and other mental health struggles have a significant impact on physical health, thereby exacerbating physical pain and illness in a vicious cycle. You have the opportunity to help your clients recognize and break these cycles, and then rebuild healthy alternatives that can promote their overall physical and emotional wellbeing.
The unique role of therapists
This introductory article is just the tip of the iceberg when it comes to the mental health impacts of living with chronic pain. Unfortunately, so many people who live with chronic pain are suffering in silence and isolation, struggling to keep their heads above the icy waters. Due to the sensitive and critical role of therapists in the chronic pain experience, you can be the life boat that steers your clients towards safety and solid ground. In a society that shapes and judges people based on their external appearances and abilities, you can help your clients rebuild their lives from the inside out. Your professional tools and knowledge enable you to understand the deep impact of pain and trauma in a way that other people do not. This support will help your clients develop the inner strength they need to resolve their relationships, rebuild their identities, and reclaim agency over their lives. And when times get rough, they know they have someone to fall back on who understands and accepts them – no questions asked.